The lichen zyberus is a disease of unknown cause, manifested by pink rounded eruptions on the skin of the body, arms and legs.
The disease is non-communicable, that is, it is not transmitted from person to person. There is no specific treatment. Passes by itself. Examination - by a dermatologist.
ICD 10 code: L42 - Pityriasis rosea. According to the classification of lichen giber refers to papulosquamous skin diseases.


The etiology (cause) of rosy lichen in humans is still unknown!
There are hypotheses of the occurrence of this skin pathology in humans:
- viral nature (herpes virus, SARS),
- infectious-allergic nature (allergic processes running after infectious diseases).
- decreased immunity is a major factor in the development of the disease,
- infectious diseases,
- avitaminosis,
- fasting, malnutrition,
- stresses
- hypothermia
- frequent use of scrubs, hard washcloths for the body.
The incidence of rosy lichen is noted mainly in the cold period of the year.
Symptoms and clinic
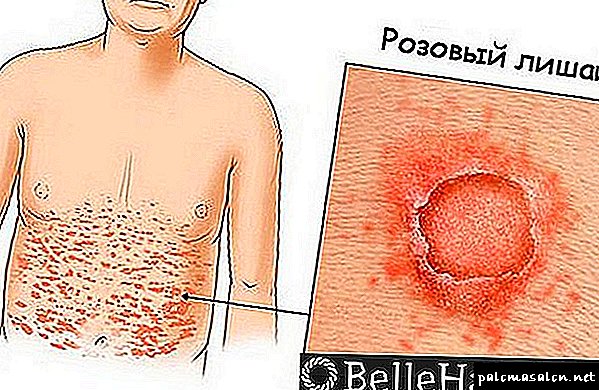
1) Maternal plaque (see picture) is an important sign of the initial stage of the disease.

- A rounded redness appears on the skin in the form of a spot of 3-5 cm in size. Usually, several days before the maternal spot appears, patients notice fever, malaise, joint pain, enlarged cervical lymph nodes - all symptoms as with ARVI.
- Maternal plaque slightly raised above the skin.
- After a few days, the maternal stain begins to peel off over its entire surface.
2) Child spots - the main symptom of pink depriving a person.


- After 7-10 days from the appearance of maternal spots, multiple pink spots ranging in size from 5 mm to 2 cm appear on the skin of the chest, abdomen, back, arms and legs.
- Spots round or oval, do not merge into conglomerates, raised above the surrounding skin. After a few days, the skin in the center of such a spot becomes pale yellow and begins to peel off. After a few more days, the central part of the spot is peeled off and the skin becomes similar to "tissue paper".
- On the periphery, the stain does not peel off, it remains pink.
- Between the central and peripheral parts of the spot remains a peeling rim (a symptom of a "collar" or "medallion").
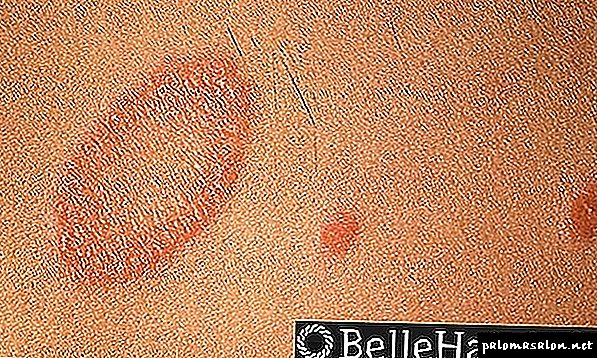
- On the body spots are located along the folds and lines of skin tension (Langer line). This symptom is considered diagnostic - it helps to establish the diagnosis.
Spots are accompanied by slight itching. This is not the main symptom of the disease; it occurs in only half of the patients. Most often, the skin itches in children and young people with an emotional psyche, as well as skin irritation.
Usually pink lichen spots do not bleed. But with severe pruritus, patients, especially children, may scratch the spots to the blood.
4) The course of the disease
- After 3-6 weeks of pink lichen spots begin to fade in the center. Spots become annular. Then the peripheral part of the spot disappears.
- For some time after the disappearance of the spot, there remains an area of increased (or vice versa - reduced) pigmentation of the skin. These pigment spots disappear by themselves within 1-2 weeks. There are no consequences in the form of scars or scars in the uncomplicated form of the disease.
- With a favorable course of recovery for a long time is not delayed, and relapse does not occur.
- The disease recurs in persons with immunodeficiency. These are HIV patients and patients with low immunity for blood cancer on the background of severe chemotherapy.
- Pink lichen may be complicated by inflammation on the skin: pustules, acne, the addition of fungal flora (mycosis). In rare cases, children may join eczematization with weeping. To avoid this, follow these guidelines.
What should not be done to the patient
- It is impossible to injure or comb spots (so that the spots do not increase in size).
- You can not rub the skin with a washcloth or even a sponge when washing in the bath, in the bathroom.
- You can not take antibiotics yourself.
- You can not sunbathe, visit the solarium.
- You can not lubricate the skin with alcohol and alcohol tinctures of iodine, brilliant green, ointments containing sulfur and tar, tar soap, salicylic ointment, apply cosmetics on the affected skin.
- You can not wear synthetic and wool items (cotton only!).
- You can not wear traumatic skin things (hard bra triggers the growth of spots under the breast).
Diet with pink lichen
1) To exclude from the diet allergenic and irritating foods:
- sweet, honey, chips, soda,
- chocolate, coffee and strong tea,
- citrus,
- artificial food additives and flavors,
- alcohol,
- smoked meat
- pepper and other spices,
- fatty foods
- pickles and marinades,
- the eggs.
2) You can and should include in the diet:
- Porridges from natural cereals: oatmeal, buckwheat, millet, 5 cereals, 7 cereals, etc.
- Bread Borodinsky, Suvorovsky, Yield, from coarse flour.
- Boiled meat.
- Potatoes, carrots and other vegetables.
Is it possible to wash?
Yes, you can, but not every day and only under the shower. You can not wash under hot water - only under warm. Washcloth not to use. Do not use soap. Dab the skin with a towel (do not rub!).
How long will the pink lichen pass?
The standard course of the disease is 10-15 days.
What to do if the rash does not pass more than 2 months?
You should consult a dermatologist for further examination for the presence of another skin disease, masquerading as Ziber иб s lichen. Most often it is necessary to exclude parapsoriasis - this will require a biopsy of the skin.
Diagnostics
The diagnosis is made on the basis of anamnesis (medical history), clinical symptoms and the exclusion of other diseases.
Laboratory diagnosis does not give characteristic signs of pink lichen (remember that the cause of the disease has not been established).
Ziber zoster has to be differentiated from a number of skin diseases:
Treatment and Prevention
In 90% of cases, treatment is not required. The patient is not contagious.
Pink versicolor passes on its own within 4-6-8 weeks after the appearance of the first spot.
Remember: if you want to quickly get rid of depriving Giber, you will not succeed. It takes time for the person’s immunity to start the fight against the disease. And for this it is necessary to remove all the provoking factors, so that the immune system quickly deal with the disease.
Drug treatment is prescribed for severe pruritus and complications.
- Antihistamine tablets: loratadine, suprastin, claritin, etc. Take the instructions (1-2 tablets per day). These drugs help to reduce allergic reactions in the body as a whole, which relieves itchy skin. Patients stop itching.
- Calcium gluconate tablets: also with antiallergic purpose (1 tablet 2 times a day).
- Ointments and creams with hydrocortisone: Flucinar ointment, Lorinden ointment, Akriderm ointment, Beloderm cream, Lokoid cream, Celestoderm ointment.
Lubricate the affected skin 2 times a day. The mechanism of action - reducing allergic reactions in the skin, edema, reducing pruritus, anti-inflammatory effect. - Ointments and creams with naphthalan oil: Naftar. The mechanism of action is the same: reduction of pruritus and inflammation in the skin. Compared to hormonal ointments, there are no such side effects.
- Antibiotics. Appointed only for complications in the form of pustular inflammation of the skin. In case of disease recurrence, antibiotics of the Erythromycin group in tablets are also included (in severe cases, injection forms in injections and hospital treatment). Previously, antibiotics were used at the onset of the disease, but now it is not recommended.
- Zindol suspension (zinc oxide) - dries the skin and reduces inflammation. It helps many patients relieve itching and skin irritation. Apply Zindol on affected skin with a cotton swab 2-3 times a day. Do not rub!
Prevention is needed to prevent the spread of the rash to other parts of the body, to prevent complications (see what the patient should not do).
Attention: Acyclovir with pink lichen does not help. Acyclovir is a medicine for the treatment of shingles (the cause of which is the herpes virus).
Folk remedies
At home, to treat pink lichen can and should be traditional medicines. Given the unclear cause of the disease, folk remedies for lichen pink have a weak effect. The same methods help someone quickly, others do not help at all, and in others they lead to deterioration.
For the treatment of pink lichen in the people use the following herbs (according to reviews of the patients themselves): celandine, string, aloe, nettle, chamomile.
- Broths celandine, succession, chamomile, burdock, etc. Broth water (do not rub or rub, but only water) the affected skin. Do not blot with cloth - let it dry by itself.
- You can not treat the skin with pink lichen alcohol tinctures in order to avoid the spread of spots on the skin.
- Do not rub wheat flour and dough.
- Do not lubricate with vinegar, sea buckthorn oil, tar, sulfuric ointment, iodine.
- It is impossible to rub newspaper ashes.
- Do not attach plants as compresses.
Inside - to strengthen the immune system:
Pink lichen during pregnancy and lactation
The lichen of Giber does not affect the fetus or the woman’s labor. Therefore, in pregnant women, this disease can not be treated with medication, but only follow a diet and gentle regimen for the skin.
When breastfeeding, the baby will not get rosy lichen.
How and what to treat?
Treatment of pink lichen in pregnant women is carried out only with severe itching and with severe inflammation of the skin.
Of the local drugs used only Zindol or talker (zinc + talc + glycerin). Corticosteroid ointments - only according to strict indications in extremely rare cases. When prescribing such ointments, breastfeeding should be discontinued.
Preparations for ingestion and injections are rarely used and should be prescribed by a doctor according to strict indications in the event of a life threatening mother.
Pink lichen in a child
Children are ill from about 4 years of age, but more often - adolescents (hormonal changes in the body, reduced immunity). The child is not contagious to others.
In children, pink lichen spots should be carefully differentiated from infectious diseases - measles, rubella.
How and what to treat?
Treatment in 90% of cases is not required. The most important thing in treating children is keeping a low-allergenic diet and preventing the spread of blemishes on a child’s skin, as children often comb and injure affected areas.
For severe itching, Zindol and antihistamines are prescribed (Claritin in syrup). If symptoms are accompanied by eczematous phenomena, in rare cases, corticosteroid ointments and creams are prescribed in a short course (Beloderm cream, etc.).
Pink versicolor

Zhiber's tinea versicolor is a mycosis, that is, a fungal infection. But this is an unusual fungal infection.
The fact is that our body is not sterile. There are many microorganisms that inhabit our body and a sufficiently large number of them lives on the skin.
Is it scary? Of course not, because the normal microflora of the skin (which includes streptococci, staphylococcus, and estericia if there are enterobacteria and many more) helps in the formation of a lipid film that protects our skin from various chemical, physical and biological traumatic factors. The change in the quantitative or qualitative composition of the microflora is called dysbacteriosis (dysbiosis) of the skin.
Localization and prevalence
Pink lichen on the body is localized mainly in the upper torso. Lesions most often occur between the ages of 10 to 40 years, women get sick more often than men.
In order for Malassezia to begin to multiply, she needs special conditions, namely: increased skin greasiness and increased sweating, increased humidity, a neutral or slightly alkaline environment.
All this can be achieved by using external contributing factors: for example, high physical exertion, being in a hot climate, working in hot workshops will give increased humidity and sweating, sun baths lasting more than 20 minutes a day give a decrease in immunity and a change in pH.
Good conditions can be achieved with the help of internal factors: seborrhea, acne - contribute to additional fat formation, diseases of the endocrine glands, vegetative-vascular dystonia contribute to excessive sweating, chronic diseases of organs and systems contribute to a decrease in immunity, and therefore changes in the quantitative composition of microflora, including and on the skin, a change in pH.
Conclusion: if Malassezia has multiplied, it means either the patient leads a fungus-promoting lifestyle, or there are health problems.
Factors predisposing to the occurrence of pathology are:
- Reduced immunity.
- Stress.
- Frequent supercooling.
- Hypovitaminosis.
- Acute bacterial and viral diseases.
- Predisposition to allergies.
- Close contact with a sick person and the use of his personal belongings.
Often, a person with pink lichen begins with the appearance on the body of the maternal plaque. This round pink spot in size from 2 cm to 5 cm, the center of which turns yellow over time. Often there is a general weakness, fever and lymph nodes. After 1-2 weeks, spots of 5-10 mm in size appear around the maternal plaque. A scaling appears in the center of the lesions, a reddish rim appears on the periphery. There is a slight itch. The formation of small spots without maternal plaque occurs less frequently.
Maternal plaque with gibere's pink lichen
3-4 weeks after the onset of the disease, the spots become brown-brown and begin to peel off, after 3-4 weeks they disappear. With constant skin irritation, the lichen pink can turn into an atypical shape. It is characterized by a bubble rash and a chronic course. Such complications arise due to frequent washing of the lesions with a washcloth and the application of irritating substances (sulfuric ointment, tar) on them.
Prevention
Primary prevention is absent. To prevent the transition of the disease to an atypical form until the complete disappearance of symptoms should be avoided:
- Bathing and using skin dryers.
- Long stay in the sun.
- Wearing synthetic and natural wool.
- Combing and rubbing lesions.
- Eating spicy, smoked, and pickled foods, alcohol, coffee, honey, eggs, fish, chocolate, and citrus.
First, to adjust the lifestyle so that the conditions on the skin do not change, so that there are no conditions for the growth of the fungus, if there are diseases that contribute to mycosis - to cure them
Secondly, the skin itself is treated with antifungal, exfoliating and pH-normalizing drugs. Treatment by a dermatologist is prescribed individually for each patient.
Do I need to disinfect laundry?
In general, versicolor versicolor is considered little contagious. As I wrote above, this pathogen lives absolutely in all people in small quantities, and only those who have certain conditions on the skin acquire leopard color. Therefore, from such people it is very difficult, almost impossible, to contract multiple-colored lichen.
But the person who is sick, you need to wash and iron your underwear and bed linen with a hot iron on both sides or boil. Because he has all the conditions on the skin for colonization and reproduction of Malassezia, and, in contact, with this raw clothing and underwear, this person will infect himself.
It took more than 2 weeks from the start of treatment, but the specks remained. Why?
If the patient was properly treated, then there will be no Malassezia on the skin surface after 2 weeks.
BUT! The fact is that fungal specks do not allow enough sun to evenly tan the skin. When the fungus disappears beneath it, unburned skin remains, there is a feeling that the patient has not recovered. You just need to wait until the skin color is equal.
If I sunbathe, skin color equal?
If the same amount of ultraviolet penetrates the skin on the tanned and unburned areas, then the amount of newly produced melanin in both areas will be the same. Consequently, the tan will be more intense, but will remain the same uneven. It is better to wait a couple of months when the upper skin cells peel off, and the color becomes even. Then the new tan will be beautiful.
Will the disease now recur?
No, if there are no contributing factors.
Yes, if you treat only the skin and do not pay attention to the other external and internal factors described above.
If I’m more than 15 years old, and I want to recover for the first time, can I be?
Yes, please contact you.
Can I give birth in the diagnosis of a multi-colored versicolor in a regular hospital, or only in an infectious?
Lichen-colored versicolor is a fungal infection of the skin that is not contagious and isolation is not required for this disease. You can give birth in an ordinary hospital.
Is it possible to cure tine lichen during pregnancy or breastfeeding, when most antifungal agents are prohibited?
Yes you can, there are weak means that are not absorbed into the skin, and which can be used during pregnancy and feeding.
Can a versicolor versicolor be passed on from me to a child?
No, versicolor versicolor is not a hereditary disease.
Finally, I will answer the philosophical question: Is it a disease or a cosmetic nuisance?
In my opinion, neither one nor the other, versicolor lichen is just an indicator, a bell that a person does something wrong somewhere, hurts his health somewhere, somewhere there are health problems, and that it is time to stop in the race of life and pay attention to yourself loved one.
Causes and symptoms of the disease
Pink lichen is classified as a dermatological infectious disease. The reasons for its development are not exactly known to doctors, but experts are inclined to believe that the symptoms of depriving Ziber in a person manifest themselves against the background of weakness of immune forces, after viral or colds illnesses that had been transferred not so long ago, as a result of overcooling of the body, or after exposure to harmful factors (harmful conditions labor, poor environmental conditions, etc.).

To this day, science has not studied whether pink lichen is contagious. If it is contagious, it can be transmitted in several ways:
To determine the onset of the disease can be on the symptoms. The initial sign of the development of the disease is the appearance of a "maternal spot" on the surface of the skin in humans. The size of the "plaque" can be different - from a few centimeters to the size of an iron coin.
After 7-10 days on the patient's body (on the extremities, back, abdomen, neck thighs) similar spots, but smaller, begin to appear (“mothers”). The color scheme of "kids" can vary from light yellow to bright pink.
The surface of the "kids" flakes and itches, which brings a person noticeable discomfort. The skin rash, as a rule, does not deliver the painful sensations.

The main difference in depriving of other types of dermatological diseases is the location of the rash - the rash is mainly located on the lips, shoulders, on the sides of the body.
The development of pink lichen negatively affects the human body. In addition to the skin rash, the patient has other symptoms:
- general malaise,
- slight increase in submandibular lymph nodes,
- temperature rise to 37-37.5 degrees.
Timely treatment of pink lichen on the body will help to quickly. Drug therapy to eliminate signs of pink lichen, as a rule, does not apply.
Effectively and quickly enough to get rid of the "spots" on the body will help folk recipes. If untreated, the symptoms of the disease are self-eliminated after 6-9 weeks.
Tips and tricks
Effectively treatment of pink lichen folk remedies. But in the process of self-treatment it is impossible to comb the “plaques”, otherwise it can lead to the introduction of a bacterial infection.
If an infection joins the disease, then therapy with folk remedies will already be ineffectual, in this case, anti-bacterial drug therapy will be required.
For the quickest treatment of rosy lichen, it is recommended to observe the following:
- For the period of therapy, you should refuse to visit the bath, sauna, bath, shower. As a body hygiene, body rubbing with warm water is used. You can not wet the "plaques" with water, soap with soap or shower gel,
- It is not recommended to use cosmetic body creams. For the period of treatment it is important to refuse to visit massage rooms, beauty salons, a swimming pool, a solarium,
- Useful for the body to wear clothes only from natural fabrics. This advice should be followed both during and after therapy,
- It is necessary to organize the correct menu, in which there will be no products-allergens. Dairy, salty, canned, pickled, spicy foods are removed from the patient's diet. It is forbidden to drink carbonated drinks and alcohol. It is necessary to limit the use of sweet dishes and sea fish.
In the room where the patient lives, the following procedures should be carried out daily:
- ventilation,
- quartz,
- wet cleaning.
Pink lichen to iodine can only be at the initial stage of the disease. According to the recommendation of a specialist, the main methods of treating pink lichen are determined.
Getting rid of itching
Folk remedies for pink lichen help get rid of the symptoms of the disease. If the “plaques” are treated with special means, then other methods can be used to eliminate itching on the body:
- Broth buckwheat. Cook in 1 tbsp. water 0.5 tbsp. buckwheat groats. The resulting decoction several times a day to wipe itchy "plaques".
- Yeast dough. Roll out a small portion of the yeast dough into a tortilla and attach it to an itchy place on the body. Keep off 30 min. up to 2 hours.
Methods of healing "plaques" with rosy lichen include the following folk remedies:
- process “plaques” with sea buckthorn oil or dog rose oil,
- apply compresses on the surface of “plaques” on the basis of St. John's wort broth,
- wipe the inflamed places with ointment prepared from 1 tbsp. l calendula flowers and a small amount of vaseline,
- apply a compress of grated beets and a small amount of honey to the "spots" for 1-2 hours.
How else can you get rid of pink lichen
For the treatment of pink lichen can be used medicines and popular recipes. At home, the doctor prescribes the following medications for the patient:
- with increasing temperature regimes of the body - antipyretic drugs (Nurofen, Paracetamol),
- with the painful itching of "stains" - antihistamine ointments or tablets (Zyrtec, Suprastin, Fenistil, Claritin),
- when introducing a bacterial infection, antibiotics (the choice of antibacterial agents is done by the doctor),
- to mitigate the severity of "plaques" - hormone-containing ointments (1% hydrocortisone, 0.5% prednisolone, 1% betamethasin).
To activate the body's resistance to the patient, antiviral drugs and vitamin-mineral complex are indicated.
Short description
Pink versicolor (pitiriaz pink, Gilbert's disease, flaky roseola, pityriasisrosea) - this acute inflammatory skin disease, presumably infectious-allergic and viral, characterized by the appearance of a common erythematous-squamous rash, seasonality (mainly in autumn and spring) and a tendency to spontaneous resolution.
INTRODUCTION
ICD-10 code (s):
Date of development / revision of the protocol:2017 year.
Abbreviations used in the protocol:
Protocol users: general practitioners, pediatricians, general practitioners, dermatovenerologists.
Patient category: adults, children.
The scale of the level of evidence:
Causes and transmission routes
It is not completely known whether it is correct to consider the causes of lichen deprivation:
- abnormalities in the epidermis due to injury,
- reduction of body defenses (immunodeficiency, chronic diseases, insufficient content of vitamins and minerals),
- psycho - emotional overload (stress, depression, mental illness),
- allergies (external irritants provoking an allergic reaction to food, household and cosmetic chemicals, drugs),
- the introduction of viral and fungal infections (frequent colds during the period of change of the year, hypothermia and overheating, chronic mycotic processes in the period of relapse),
- flea bites, lice, bedbugs.
Undoubtedly, all of the above factors individually or collectively have their own significance. But, with a high degree of confidence, the research confirms that Zhiber ’s lichen pink has the etiology of viral origin, as in the vast majority of tests taken at the peak of symptoms, traces of herpes viruses have been found.
Doctors accurately determined that zyber's pink zoster is not transmitted to humans from animals. And, since the reason is not known, the ways of transmission are not entirely clear. Experts recommend beware or exclude:
- close direct contacts with the sick (kisses, hugs, intimate relationships),
- use of personal hygiene items affected (towels, combs, scourers, underwear and clothing).
Pink lichen - the main symptoms
As with other types of lichen, with pink lichen, the main distinguishing feature is a rash, which has its own characteristics. In the photo you can carefully consider the symptoms of pink lichen.
Pink versicolor begins with the appearance of the "maternal plaque" - one or more single spots of intense pink hue. They have bright, clear contours that resemble the shape of a medallion. The diameter of the rash is balanced in values from 2 to 5 centimeters.

In the center of the plaque skin tone becomes yellowish. The skin is dry, with exfoliating scales. Many note itching, less often - formation of bubbles and a burning sensation. If a patient has a severely weakened immune system, the vesicles may merge into larger vesicles.
Against the background of deterioration of health, the temperature periodically rises, weakness is noted, in some cases - an increase in lymph nodes in the neck and under the lower jaw.
There is a distribution of specks in the form of small foci. Pink lichen "loves" to localize along the line of Langer (invisible lines of the body, located across the fibers of the muscles). On the body, they are usually located in places of natural skin folds on the shoulders, sides of the body, back, and hips. The overall pattern of plaques remotely resembles the distribution of spruce branches along the trunk.
Update rash occurs two to three weeks from the onset of the first symptom. At this time, pink versicolor is characterized by the presence of both old foci and new ones.
The duration of the flow is from one to six months. After this period, the symptoms subside or disappear altogether.
Pink versicolor is only acute and never becomes chronic. A person who has had this disease gets a lifelong immunity to it.
The disease can give complications. As a rule, these are vesicles with transparent contents (a very rare individual feature), combing which turns into purulent inflammation, that is, to cause the addition of a bacterial infection.
Pink lichen on the head
Sometimes pink versicolor affects the scalp. At the same time it is characterized by:

- the appearance of separate oval spots, with clear outlines,
- constant scratching,
- hair loss.
The disease in this manifestation is quite rare. However, its duration (in case of occurrence) is sometimes delayed up to three months.
Pink versicolor in women during pregnancy
Waiting for a child for a woman is a difficult and uneasy time. Restructuring to carry a baby forces the body to work for two. Hormonal vigor shakes up the nervous and immune systems. In future mothers, the metabolism is changing, various allergic reactions are possible. At this time, the disease can easily "attack" the body of a pregnant woman.
However, you shouldn't worry too much. If the doctor's prescriptions are followed during the course of treatment, as well as the personal hygiene rules, the lichen pink will quickly recede.
The main thing - to miss the handful of pills and not to succumb to the provocative advice of girlfriends.
Pink lichen in children
Deprive "clings" to children, especially those who often have colds and are prone to allergies.
Symptoms of the disease in children:
- weakness and malaise
- headache and pain in the joints,
- slight temperature rise
- itching at localized foci,
- lack of appetite,
- bad sleep
- enlarged submandibular lymph nodes.
Babies get sick less often. A good barrier to the penetration of a disease-causing principle exposes breast breast milk.
Kindergarten children (especially during the period of adaptation in the children's team), as well as adolescents (during hormonal adjustment at a difficult transitional age) get sick much more often.
Rash in children affects areas of sweat gland concentration throughout the body:
- on the sides under the arms and on the back,
- in the groin and abdomen,
- on the upper and lower extremities (forearms and thighs),
- less often on the neck and face.
Children usually tolerate pink versicolor more easily than adults - the disease most often goes away by itself, even without treatment. However, parents still have to consult a doctor for advice.
When the diagnosis is confirmed, symptomatic treatment is prescribed to speed up recovery.
Terms and Definitions
Zyber's pink versicolor (Pitirias pink, Ziber ’s disease, flaky roseola, pityriasis rosea) is an acute inflammatory self-resolving dermatosis, characterized by typical oval or monomatous spotty-papular and erythematous-squamous foci, primarily located on the trunk and proximal forms.
How to cure pink shingles at home?
It is quite simple to treat pink lichen at home. It is enough to exclude irritation of the skin and not consume products that may cause allergies. However, before you begin treatment, be sure to consult a doctor. Even if your symptoms fully fit the description of the disease, it does not mean that you can properly diagnose yourself. There are at least five other diseases with similar manifestations.
If a dermatologist has determined that you have a pink lichen, then the following measures should be taken:
- Change your underwear daily. You can only wear cotton. Bed linen should also be made of natural fabric.
- Wear loose clothing. If possible, give up tight things, including linen. These are wide T-shirts with short sleeves; if the weather permits, men are better off walking with a naked torso. Try to ensure free access of air to the affected skin.
- Take a warm shower no more than 1 time per day. Wash affected areas without soap. Do not use washcloth. After a shower, do not rub the skin, but lightly dry it with a clean towel. Doctors of the old school recommend not to wet the affected areas, but Western medicine does not impose such restrictions.
- Avoid situations in which excessive sweating occurs: active sports, warm clothes made of synthetic materials.
- Avoid stress. The active release of adrenaline can cause itching and the appearance of new rashes.
- Consult a doctor about hormonal corticosteroid ointments.. They are applied only on the itchy elements of the rash with a thin layer: Akriderm (2 times a day), Advantan (1 time a day). Drugs use no more than 2 weeks.
- Antihistamines have a pronounced antipruritic effect - Suprastin (2-3 times a day), Allertek (10 ml 1 time a day).
 Enterosorbents (White coal, Polysorb, Enterosgel) cleanse the intestines and blood from allergens and toxins, thereby improving skin condition.
Enterosorbents (White coal, Polysorb, Enterosgel) cleanse the intestines and blood from allergens and toxins, thereby improving skin condition.
Recall that each of the drugs has a list of contraindications, so only a doctor can prescribe and determine the dosage.
As you know, there are theories about the infectious-allergic and viral nature of the disease. On this basis, attempts are being made to cure pink lichen:
- immunomodulators - Recombinant alpha / gamma interferons, Kagocel,
- antiviral drugs - acyclovir, geviran,
- antibiotics - Erythromycin, Azimed.
However, dermatologists do not recommend the use of these drugs. Immunostimulants increase the risk that allergies will increase, causing the rash to spread. Antibiotics and antivirals, which supposedly accelerate recovery, are ambiguous. Reliable research on this issue was not conducted, therefore, these drugs are usually not prescribed.
Pink versicolor does not violate the performance, and with this diagnosis does not give sick leave. You can go to work, and in the meantime, cure pink zoster at home.
Pink lichen during pregnancy. What to do?
 Pink versicolor during pregnancy - a fairly common phenomenon. High incidence, compared with other groups of the population, is associated with hormonal disruption and a natural decrease in immunity during this period of a woman’s life. The disease itself is not dangerous for the health of the mother and child, and does not threaten the pregnancy, however, severe itching and the associated nervous tension aggravate the condition of the woman. In this regard, if the pink lichen developed before the 15th week, the risk of miscarriage increases.
Pink versicolor during pregnancy - a fairly common phenomenon. High incidence, compared with other groups of the population, is associated with hormonal disruption and a natural decrease in immunity during this period of a woman’s life. The disease itself is not dangerous for the health of the mother and child, and does not threaten the pregnancy, however, severe itching and the associated nervous tension aggravate the condition of the woman. In this regard, if the pink lichen developed before the 15th week, the risk of miscarriage increases.
What to do if the doctor diagnosed lichen pink during pregnancy?
- Vitamin therapy - vitamins A, C and all the representatives of group B. They strengthen the immune system and speed up recovery. Vitamins are taken in the form of vitamin complexes (Pregnavit, Additive) or separately.
- Calcium gluconate contains calcium salts that improve the state of the musculoskeletal system of the mother and fetus, which have antiallergic, hyposensitizing effect. Calcium gluconate reduces the permeability of blood vessels and cell membranes, thereby preventing the development of inflammatory and allergic reactions on the skin. Take 1 tablet 3 times a day for 2-3 weeks.
- Phototherapy - exposure to an ultraviolet lamp or short-term (15-20 minutes) exposure to the sun. UFO strengthens the immune system, improves skin condition and kills pathogenic bacteria.
- External treatment of pink lichen in pregnant women:
- The oil solution chlorophyllipta - has antimicrobial properties and accelerates regeneration, has a softening effect. Lubricate the lesions 1-2 times a day with a solution.
- Sea buckthorn, peach, rosehip oils - contain vitamins, flavonoids and fatty acids, which have an anti-inflammatory and regenerating effect, soften the skin, reducing itching. Gauze cloth moistened with oil, applied to the lesions for 10-15 minutes, 2 times a day.
- Zinc ointment - reduces inflammation and irritation, forms a barrier that prevents the penetration of bacteria and infection of the lesions. Apply 2-4 times a day on the affected skin.
- Advantan cream is a "hormonal" corticosteroid agent that reduces itching, burning and other manifestations of lichen rosacea. Apply with caution, only as prescribed by a doctor 1 time per day, not more than 4 weeks.
When treating pink lichen during pregnancy, it is important not to overload the body with medicines that may be more dangerous than the disease itself. Based on this, many doctors advise to eliminate all medications, allergens, local irritants and wait for the disease to disappear itself.
What is impossible with pink lichen?
Dermatologists acknowledge that there is no effective medical treatment that would suit all patients. However, if we exclude everything that is impossible with rosy lichen, the manifestations of the disease will disappear in 1-2 weeks.
With pink lichen is undesirable:
- Often take water treatments. Wetting causes the appearance of new foci of pink lichen. Why this happens, it was not possible to install. However, doctors recommend taking a shower no more than 1 time a day.
- Use washcloths and detergents. The bast leaves microscopic abrasions on the skin, in the place of which new foci appear. Substances that are part of soap and shower gels cause allergic reactions, which also increase the rash.
- Attend the pool. Bleach used to disinfect water can cause a rash to spread.
- Sweat. Salts that are part of the sweat, are irritating to the skin, so excessive sweating contributes to the appearance of "daughter" lichen spots. It is recommended to exclude situations when a person actively sweats: intense exercise, warm clothes that are not suitable for the weather.
- Combing spots. Bacteria get into microscopic abrasions, and secondary infection joins pink lichen, which significantly complicates the course of the disease.
- Use ointment with tar and sulfur. These substances dry the skin, increasing itching.
- Massage. This procedure enhances the blood flow to the skin. Because of this, the rash becomes more visible. In addition, during massage the skin is stretched and injured, which increases the risk of infection.
- Wear woolen and synthetic clothing. Wool "bites", irritating the skin. Synthetics do not absorb sweat, its salts and moisture create favorable conditions for the growth of bacteria. These tissues often cause the spread of rashes.
- Wear tight clothing. Lingerie and things that fit snugly to the body rub skin during movement. Especially often this occurs in places where the skin is in contact with the seams and elastic bands of linen. On these scuffs and abrasions, an inflammatory reaction is triggered, and new lesions appear.
 Take baths, go to baths and saunas. High humidity and high temperatures cause dilation of blood vessels in the skin and increase the secretion of blood vessels through its surface. This process always ends with the spread of the rash.
Take baths, go to baths and saunas. High humidity and high temperatures cause dilation of blood vessels in the skin and increase the secretion of blood vessels through its surface. This process always ends with the spread of the rash.- Supercool. Low temperatures cause a spasm of blood vessels in the area that has been subjected to hypothermia and weaken the immune system.
- Smear the skin with alcohol tinctures. Alcohol dries the skin, thinning its protective layer (hydro-lipid mantle). Any irritation of the skin with aggressive substances, which include alcohol solutions, is highly undesirable in case of pink lichen.
- Use cosmetics for the body. Cosmetics ingredients dry the skin, therefore complicating the release of toxins. In addition, they are allergens.
- Sunbathe. Sunburns, like other skin damage, trigger a cascade of inflammatory reactions that underlie the appearance of foci of the disease. However, ultraviolet light in moderate doses is useful for patients with rosy lichen. Recommended to stay in the sun for 15-20 minutes a day from 8 to 11 or from 16 to 18 hours.
- Consume allergenic products - salty, smoked, spicy, as well as dishes containing many food additives (chips, crackers) and alcohol. They increase the production of histamine, which triggers an allergic reaction.
Risk group
Pink lichen is not considered a contagious disease, as people can contact patients for years and not be infected. But you can “catch” the disease in 5 minutes, if the body's immune forces are weakened.
Women suffer more often than men, the age group of risk is 10 - 40 years. The factors that cause skin disease are manifold, but they are all associated with low immunity. The following causes provoke the formation of pink lichen on the skin:
Sometimes infection occurs on the background of allergies, anemia, vitamin deficiency. In some situations, close household contacts are the cause.

How does deprive pink in people, symptoms (signs)
Independently, guided by publications on the Internet, it is impossible to diagnose pink lichen with extreme precision. A lot of diseases have similar symptoms, for example, secondary manifestations of syphilis, so be sure to go to a dermatologist. Characteristic symptoms of pink lichen in a person:
- fever, weakness, muscle pain, in some cases, inflammation of the lymph nodes, fever,
- a large pink spot (called the physician's mother) with a diameter of 1 - 5 cm, in the chest, neck or back. Over time, it turns pale in the center, and begins to peel off, and around the circumference is pink and smooth, visually reminiscent of a medallion,
- antihistamines - Suprastin, Diazolin, Erius, Claritin, Tavegil, others.
- Calcium gluconate,
- Calcium chloride.
- Chatters oil or water-alcohol solutions with powders.
- Multivitamins.
- Broad-spectrum antibiotics Erythromycin, Tetracycline.
- Antifungal, antibacterial ointment Sanguirytin.

Usually the painful condition lasts 6 to 9 weeks, the rash disappears without the use of drugs.
It is possible that pathogenic bacteria infect the sites, purulent foci of inflammation occur, then medication is not necessary.
Pink lichen can occur with complications: against the background of general intoxication, the formation of new, highly itchy, rash occurs, then the disease lasts up to six months or more, with constant relapses. Serious complex treatment will be required.
Treat pink zoster in a person or forget how to do no harm: ointments, drugs, medications
Treatment for pink lichen in humans is made in accordance with the definition of the severity of the disease.
In the case of a single rash, not exciting large areas, the treatment is aimed at increasing the body's immune forces: taking a complex of vitamins and minerals.
 If the process is long, but without complications, the doctor recommends a diet that excludes products that contribute to the formation of an allergic reaction.
If the process is long, but without complications, the doctor recommends a diet that excludes products that contribute to the formation of an allergic reaction.
When infected with purulent microorganisms, antibacterial therapy, anti-inflammatory and antihistamine preparations are prescribed for the treatment of rosy lichen in humans.
Principles of treatment of the initial stage of lichen deprivation are in compliance with important rules.
If the disease began during pregnancy, the woman should be treated by a dermatologist under the supervision of a gynecologist, since miscarriage is possible during early pregnancy.
Effective treatments
It is important to remember: people with strong immunity do not get sick, so take care of your health “from the very young.”
 If such an attack happened, as an incomprehensible rash on the body, the cause of which is Gilbert versicolor, immediately go to a dermatologist. After the examination, he will prescribe one of the methods of treatment. What medications are used to treat pink lichen in a person?
If such an attack happened, as an incomprehensible rash on the body, the cause of which is Gilbert versicolor, immediately go to a dermatologist. After the examination, he will prescribe one of the methods of treatment. What medications are used to treat pink lichen in a person?
With minor manifestations
Apply drugs to improve immunity: vitamin therapy (A, C, B, PP), calcium. If there is a slight itch - Zindol - a suspension of starch, zinc, talc, glycerin and water. Mandatory diet. Exclude cosmetics, perfumes.

With an acutely current form
Here, during a disease, pills for pink lichen in a person are prescribed:
If the child is sick: folk remedies and vitamins
At this stage, the use of medicines is minimized: vitamin Ascorutin (C and P) - to increase the immune defense, antihistamine - Finistil to reduce the intensity of itching.

An important condition for successful treatment: maintaining a favorable microclimate in the patient's room. Ventilate the room often, moisten the air, and keep it clean. Be sure to separate the towel, other items of personal hygiene. If possible, use quartz. Do not download errands, good rest, good mood - the most successful healers.
In some recipes of folk healers, there are unique obscurantism tips: "Burn the newspaper, sprinkle ashes on the plaques."
Do not try to follow such instructions, imagine what kind of rubbish you can infect a diseased area of skin, this is a direct way to the intensive care unit of the hospital.
Even an online consultation with a dermatologist may not work, as a visual inspection through the monitor does not reveal a picture of the disease. Contact the clinic.
Self deprivation of pink lichen with medications, and especially folk remedies is unacceptable, it is not known what complication this insufficiently studied disease can cause when using drugs, herbs, powders.
First of all, when a rash appears, be careful that there is no external irritation of the plaques and contact with water.
 Proper nutrition is the key to treating many ailments.
Proper nutrition is the key to treating many ailments.
When the immune defense increases, and the body adapts to internal stimuli: microbes, toxins accumulated during the disease, allergens, stress, everything that was a provoking factor, the disease will recede. Perhaps the cause of the disease is much closer than it seems - this is the composition of the products that are present in the daily menu. Chickens fed with hormones, fruits, saturated with pesticides, toxic additives that are used in canning. And the body reacts sharply to stimuli. Eat right!

 Enterosorbents (White coal, Polysorb, Enterosgel) cleanse the intestines and blood from allergens and toxins, thereby improving skin condition.
Enterosorbents (White coal, Polysorb, Enterosgel) cleanse the intestines and blood from allergens and toxins, thereby improving skin condition. Take baths, go to baths and saunas. High humidity and high temperatures cause dilation of blood vessels in the skin and increase the secretion of blood vessels through its surface. This process always ends with the spread of the rash.
Take baths, go to baths and saunas. High humidity and high temperatures cause dilation of blood vessels in the skin and increase the secretion of blood vessels through its surface. This process always ends with the spread of the rash.

